What is involved?
The operation is performed under a combination of general and regional anaesthesia. The shoulder joint is exposed and one or both bearing surfaces of the joint are resurfaced or replaced with metal and plastic implants. You will spend 1-3 nights in hospital.
What are the benefits?
A shoulder replacement renders the shoulder relatively pain free, improves the range of movements and allows better use of the shoulder and these in turn lead to an improvement in the quality of life. Some patients may achieve near-normal function after a shoulder replacement.
What are the alternatives?
Painful arthritis of the shoulder may be treated in the early stages with pain relieving medication, activity modification, physiotherapy, injections or arthroscopic surgery. If symptoms persist for a prolonged period of time despite trying some or all of these measures then joint replacement surgery may be appropriate.
What are the risks?
The overall risk of complications after a shoulder replacement is approximately 8% compared with 16% after hip replacement and 14% after knee replacement.
Medical complications
Chest infection, pulmonary embolism, myocardial infection or stroke are possible after surgery.
Surgical complications
Infection: This can occur after any operation where metal devices are implanted in the body. Several measures are employed to minimize the risk of infection including administration of antibiotics prior to the operation, an antiseptic technique and the use of a clean air theatre. The risk is 1-2%.
Nerve injury: This is possible but rare. The risk is 1-2%. Most nerve injuries recover.
Bleeding : Bleeding may occur during or after surgery. In very rare instances a blood vessel may be damaged as a consequence of injury or surgery. A blood transfusion is rarely required.
Thrombosis: Clots may develop in the deep veins of the arm or legs or rarely in the lungs. Several different preventive measure are employed during and after surgery. You can help yourself by keeping your ankles and toes moving and walking as soon as tolerated.
Stiffness: This may occur after surgery. You will be given advice on moving the shoulder by the physiotherapists and it is important you follow these instructions.
Rotator cuff failure: This is a consequence of wear and tear of the rotator cuff tendons and can occur even in the absence of injury.
Instability: The shoulder may dislocate after shoulder replacement surgery but this is rare.
Periprosthetic fracture: The bones may fracture during the course of the operation. This may necessitate delaying the rehabilitation of the shoulder.
Glenoid erosion: In patients where only the ball of the joint has been replaced, over a period of time the cartilage (gristle) on the socket of the shoulder may wear leading to pain.
Wear and osteolysis: The plastic components in joints may wear over time. This produces microscopic debris that generates an inflammatory reaction in the surrounding tissues and bone leading to loosening.
Loosening: Artificial joints may loosen due to mechanical wear over time resulting in pain.
Revision: If the artificial joint is not working satisfactorily due to pain, glenoid erosion, loosening, infection or rotator cuff failure then further surgery may be necessary to exchange the joint.
Aftercare
Following the procedure the skin incision will be closed with sutures and tape and covered with a shower-proof dressing. The dressing should be left undisturbed until the sutures are removed at 14 days. You will be shown how to start moving the shoulder by a physiotherapist. You will be provided with a sling, which may be removed intermittently to perform exercises. After 6 weeks you will be allowed to move the shoulder actively and may resume driving once you have achieved control of the arm. Strengthening exercises are started after 12 weeks or when satisfactory movements and control have been regained. Outpatient physiotherapy will be arranged and may be continued for 3-6 months after surgery.
The different types of shoulder replacement
Shoulder replacements can be broadly divided into two categories – anatomic or reverse shoulder replacement.
Anatomic Shoulder Replacement
Anatomic replacements aim to preserve the shape and orientation of the joint and rely on the rotator cuff to provide control of the joint. Anatomic replacements may include total shoulder replacement where both the ball and the socket are replaced, or partial replacement (or hemiarthroplasty) where only the ball is replaced. There are many different techniques of replacing the shoulder
Humeral head resurfacing: In this procedure the head of the humerus (the ball of the joint) is resurfaced with a metal “cap”. This provides a smooth and hard bearing surface on the ball side of the joint and may be appropriate where only one side of the joint is damaged in conditions such as avascular necrosis of the humeral head. It generally provides very good pain relief if the natural socket of the shoulder is relatively healthy. The procedure conserves bone making subsequent revision surgery less challenging.
Total shoulder resurfacing: Both the ball and the socket of the joint are resurfaced in this procedure. This is a technically demanding operation and is indicated for conditions where both surfaces of the joint are damaged such as in osteoarthritis or rheumatoid arthritis. A functionally intact rotator cuff is a prerequisite. The procedure provides excellent pain relief and improvement in function. The procedure conserves bone making subsequent revision surgery less challenging.
Stemless shoulder replacement: The ball of the joint is removed and replaced with a metal prosthesis fixed in the upper part of the bone but without a stem in the shaft of the humerus. The glenoid may or may not be resurfaced at the same time.
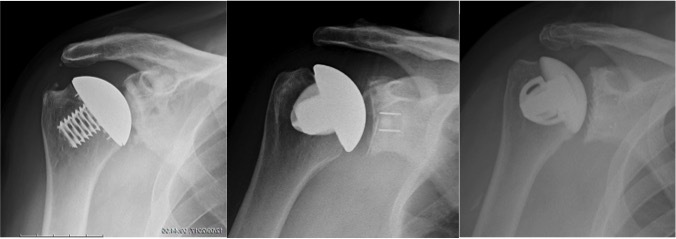
Stemmed shoulder replacement: This is the conventional type of shoulder replacement. The ball of the joint is cut and a metal prosthesis with a stem is implanted in the humerus. If only the ball of the joint is replaced the procedure is called a Hemiarthroplasty. If the glenoid is replaced at the same time the procedure is referred to as a Total shoulder replacement.
Reverse Shoulder Replacement
In a reverse shoulder replacement the orientation of the joint is changed such that an artificial ball is fixed to the shoulder blade and a socket is fixed to the humerus. A reverse shoulder replacement is used in patients where the rotator cuff is torn or deficient.
Choosing the right shoulder replacement
Choosing a shoulder replacement depends on a number of different factors. Mr Patel and Mr Little have extensive experience in shoulder replacement surgery and will advise you of the most appropriate type of shoulder replacement for your condition.