How is the procedure performed?
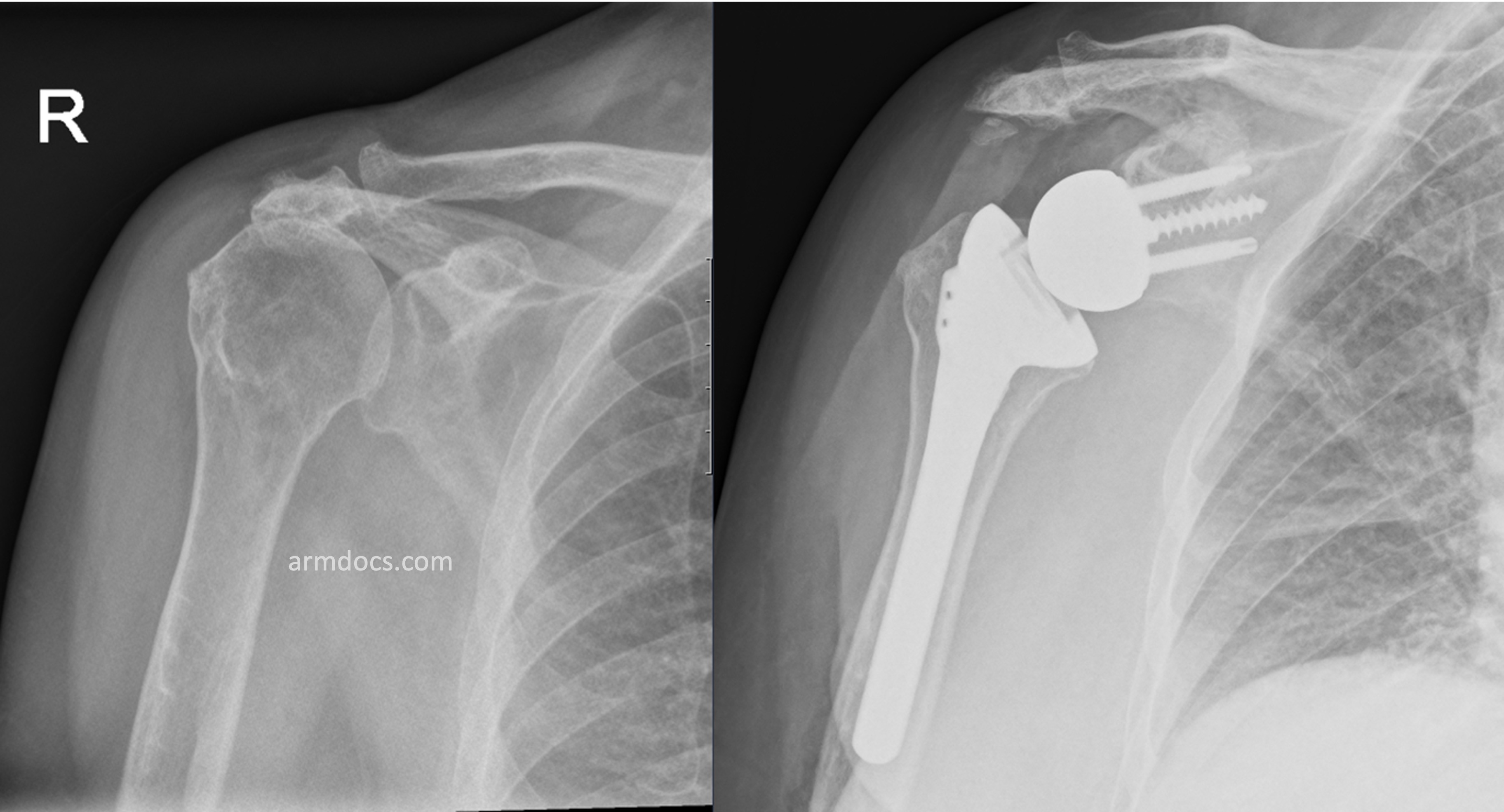
The procedure is performed under a combination of general and regional anaesthesia. The shoulder joint is exposed. The bones on either side of the joint are prepared, a metal “ball” is fixed to the native socket with screws and a “socket” on a stem is fixed to the humerus, usually with bone cement.
Benefits
The main benefit of the procedure is to relieve pain and improve the range of movements. This is often associated with an improvement in the function of the joint and ability to use the arm.
Risks
Infection (3-5 %) - Antibiotics are routinely used as a preventive measure.
Bleeding – A small amount of bleeding is inevitable but blood transfusion is rarely necessary.
Instability (4-6%) The artificial shoulder can sometimes slip out of place. This may require relocation with manipulation under anaesthesia or rarely further surgery.
Thromboembolism – It is possible to get venous clots in the arm, legs or the lungs. Preventive measures are employed during and after surgery.
Nerve injury (1-2%) - Specific precautions are taken during surgery to protect the nerves but injury to the axillary nerve is possible. In most instances this will recover on its own over a period of time.
Deltoid muscle failure – This has been reported but is uncommon.
Lengthening of the arm – The operated arm may become slightly longer after the operation.
Fracture (2-3%) – Fractures of the humerus or the glenoid may occur during or after the operation. In rare instances stress fractures of the scapular spine may occur.
Hardware failure – The metal screws can break or rarely the components can disengage.
Persistence of symptoms– Occasionally a degree of pain or weakness of the shoulder may persist for some months. If these symptoms fail to resolve, then further investigation or treatment may be necessary.
Wear and Loosening – Artificial joints can wear over time and occasionally work loose. This may lead to further surgery.
Revision – Surgery to replace the artificial joint may occasionally be required if the joint works loose or develops other problems.
Aftercare
Following the procedure the surgical incision will be closed with sutures and covered with a dressing. The dressing should be left undisturbed as far as possible for 10-14 days. If the dressing is removed for any reason this should be replaced with a similar dressing. A sling will be provided to support the arm, but may be removed intermittently as tolerated during meal times, while showering / changing and when resting. A physiotherapist will provide instructions about mobilising the shoulder prior to discharge from hospital. Outpatient physiotherapy is usually started no later than a week after surgery.
For detailed instructions on rehabilitation click here.
Resuming work, driving and activities
Office duties may be resumed within 3 weeks. Manual tasks should be avoided for at least 3 months. You may be able to resume driving at 6-8 weeks.
Follow-up
An appointment will be arranged for you to in the outpatient clinic at 2 weeks after the procedure. Further Follow-up is required at 6 wks and at 3, 6 and 12 months after surgery or until a satisfactory recovery is achieved.