What is the pathology of Shoulder instability?
A dislocation of the shoulder usually results in damage to the ligaments of the shoulder, the labrum (the “bumper”) or to the bony rim of the socket of the shoulder. The most common injury is a detachment of the anterior labrum (referred to as a "Bankart lesion"). It may also result in indentation of the ball of the shoulder (a “Hill-Sachs” lesion). Some individuals with “loose” joints may suffer recurrent instability due to their muscles working in abnormal fashion (referred to as instability due to abnormal “muscle patterning”).
How is Shoulder instability diagnosed?
A diagnosis of Shoulder instability is made based on the history of repeated episodes of the shoulder coming out of joint. Occasionally patients may experience symptoms of a “dead arm” with sporting or other activities in the absence of dislocation. Examination may show signs of laxity or “looseness” in multiple joints, pain with certain movements of the shoulder and signs of apprehension or a feeling that the shoulder may come out when placed in certain positions. X-rays are essential to look for damage to the bony rim of the socket or indentation of the ball of the joint. Special imaging with an MRI scan may be requested to obtain further information about the state of the labrum and the ligaments. In some instances an MR arthrogram (MRI scan after injection of contrast fluid in the joint) may be requested. A CT scan may be arranged to assess the damage to the bony rim of the socket (glenoid) or the ball of the joint (humeral head).
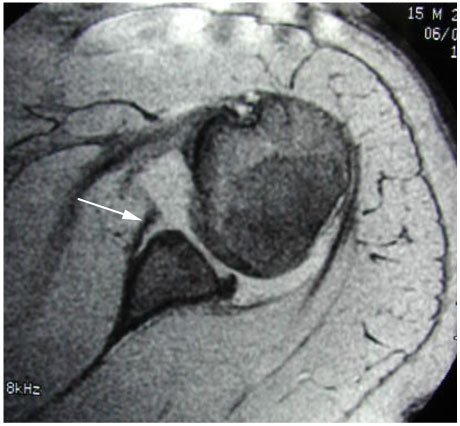
MRI showing a Bankart lesion
Is there a risk of recurrence with Shoulder instability?
The risk of recurrence of traumatic instability depends on gender and the age at which the first episode occurred. The risk of recurrence is lower in women and is greatest in young men below 25 years of age and diminishes with age.
How is Shoulder instability treated?
In the early phase, symptoms may be controlled with activity modification.
Supervised physiotherapy: You may be advised to see a physiotherapist to start a regime of specific exercises to improve scapular positioning and strengthen the rotator cuff.
The British Elbow and Shoulder Society (BESS) video on shoulder instability has useful guidance and exercises for patients with shoulder instability.
Physiotherapy is often the main treatment for patients who have developed symptoms of instability in the absence of an injury.
Braces: A specific brace for the shoulder may be used for short periods of time to protect the shoulder and get sporting individuals through to the end of a season.
Surgery: Surgery may be appropriate following a single dislocation in individuals who are at a high risk of recurrence or where an individual has suffered more than one episode of instability following an initial injury. This is a highly individualised decision and should be made after detailed discussion with a specialist surgeon. The operation performed will depend on the pathology identified on clinical and radiological assessment. It may consist of an Arthroscopic repair where the tears in the labrum and ligaments are repaired with “keyhole” surgery. In cases where there is significant bone damage to the rim of the socket or the ball of the joint, additional procedures such as a "remplissage" or bony reconstruction of the rim of the socket may be necessary.
For further information on surgical treatment, please refer to the sections on “Arthroscopic stabilisation of the shoulder” and “Bony reconstruction for shoulder instability”.